While the femoral approach is widely used in endovascular treatment (EVT), careful selection of the access site is crucial to minimize access site complications and prevent adverse outcomes. A U.S. study analyzing 27,048 interventions in 22,226 cases of femoral approach EVT found that 3.5% of patients experienced access site complications1. Among patients with severe complications, many required transfers to rehabilitation facilities or other hospitals (22.1%) or discharge to nursing homes (15.8%). Furthermore, these patients had a higher 30-day mortality rate (6.1%), highlighting the invasive nature of the femoral approach as a significant concern.
At our facility, we have long prioritized safety measures such as ultrasound-guided puncture to reduce access site complications associated with the femoral approach and to minimize patient burden. However, with the recent increase in EVT for elderly patients, we have introduced radial EVT as a less invasive approach.
The R2P™ (Radial to Peripheral) system, which enables the radial approach, can potentially reduce access site complications due to the relative ease of achieving hemostasis at the puncture site2. Additionally, it eliminates the need for post-procedural bed rest and urinary catheterization, further reducing patient burden.
However, there is a risk of complications such as stroke, abdominal vascular embolism, or intestinal necrosis if thrombi or plaque from the vessel walls are dislodged along the access route to the lesion. Therefore, pre-procedural screening is essential to confirm the absence of aortic tortuosity and to ensure there are no thrombi or plaques in the subclavian artery or aorta.
Keeping these potential complications in mind, we believe the R2P™ approach offers significant advantages, particularly in cases where femoral access is challenging.
Benefits of the Radial Approach
- Relatively easy hemostasis
- Minimal requirement for bed rest3
- No need for urinary catheterization
Applications of R2P™
- Stenotic lesions
- Absence of aortic tortuosity
- No plaques in the subclavian artery or aorta
- Cases where femoral approach is challenging
At our facility, we adhere to these key points when screening for R2P™ cases (fig. 1).
First, we evaluate the morphology of the lesion site using preoperative CT and MRA to determine whether backup support is necessary. We consider R2P™ feasible if the lesion site is characterized as SOS (Simple lesion, Open vessel, Short lesion). However, for CTO lesions, where wiring solely with R2P™ can be challenging, we employ a bidirectional access approach. This typically involves inserting a 4Fr sheath from the femoral artery to advance an IVUS catheter, while simultaneously advancing a stent from the radial artery.
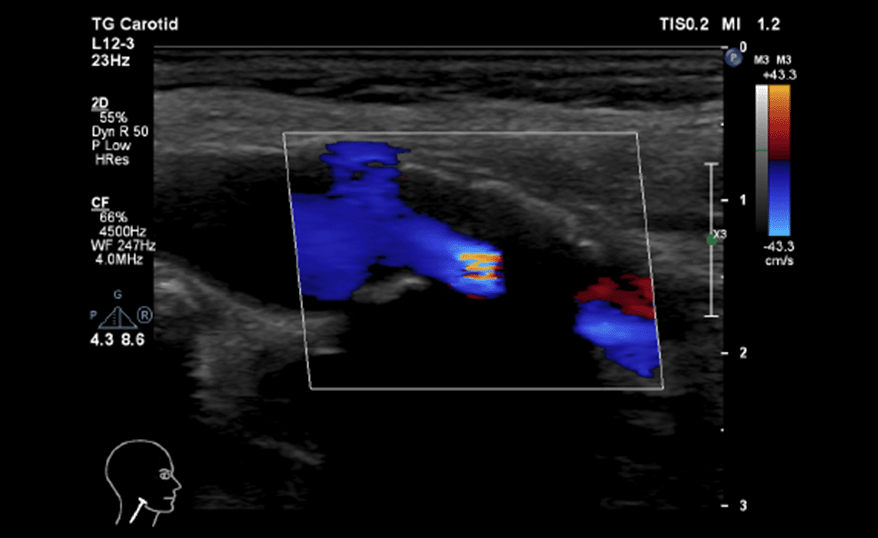
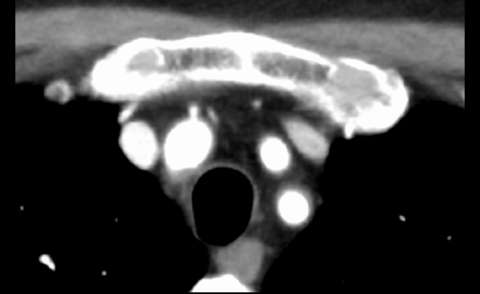
Next, we assess vascular access. While evaluation of the lesion site is crucial in the radial approach, assessing the access vessels is equally, if not more, important. We prefer the left radial approach as it typically involves fewer contact points with the aortic wall. To evaluate accessibility through the subclavian artery and aorta, we use CT and transesophageal echocardiography (TEE) to assess the condition of plaque in the surrounding arteries. We exercise particular caution when using the radial approach in cases with extensive aortic plaque or severe carotid stenosis (fig. 2). For patients with a history of stroke or in cases where a shaggy aorta is observed (as shown in fig. 3), we opt for the femoral approach.
In cases where the catheter cannot be advanced smoothly with R2P™ or when backup support is insufficient, we prepare for a retrograde approach via femoral access. The access site is selected by the patient after explaining to the advantages and disadvantages of each approach, as well as the risk of stroke.
Fig. 1: Key Considerations for Screening R2P™ Cases at Tokyo General Hospital
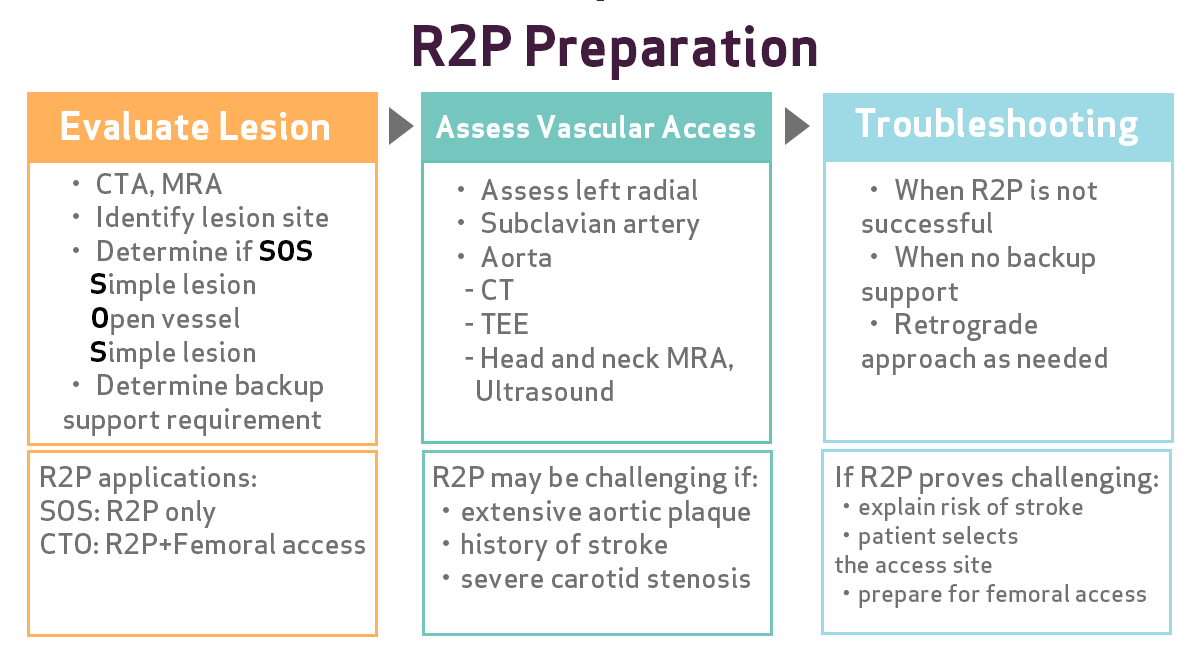
Fig. 2: Assessing Plaque Formation and Arterial Stenosis
In cases where ultrasound reveals carotid artery stenosis of 50% or greater, there is often a tendency for plaque formation throughout the aorta. In such cases, EVT via the radial approach should be performed with caution.
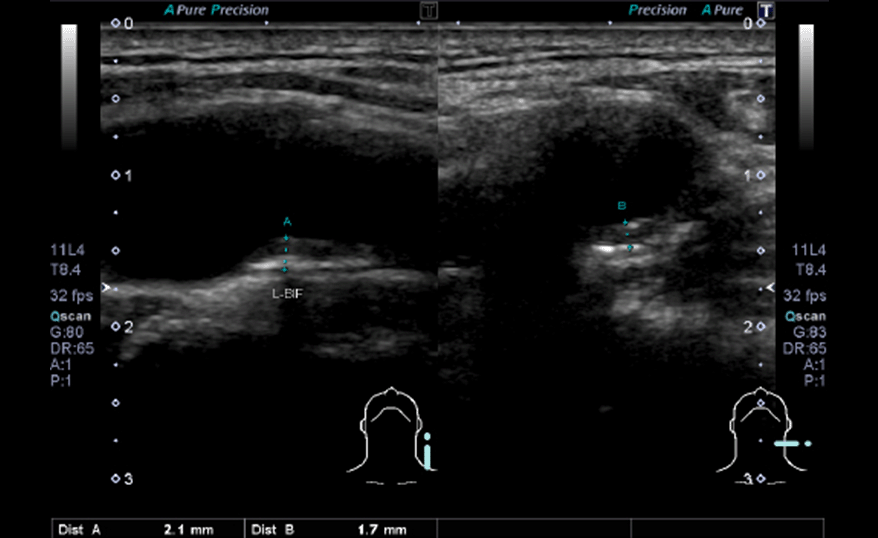
a) No plaque
b) Plaque formation throughout the aorta
Fig. 3: Aortic Evaluation Using TEE
In cases where TEE reveals a shaggy aorta on the aortic wall, we opt for the femoral approach due to the high risk of atheroma dislodgment by the catheter.
This case demonstrates an EVT performed on the iliac artery using a distal radial approach (DRA) (fig. 4). When performing DRA punctures, we consistently use ultrasound guidance to ensure safety.
Fig. 4: Evaluation of the Lesion and Access Route
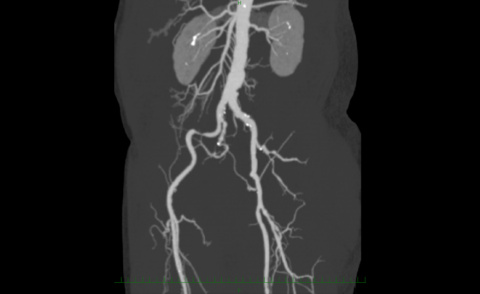
Lesion / Preoperative CT
Despite tortuosity in the right iliac artery, we determined that the Misago stent's flexibility would allow it to conform to the vessel without causing excessive straightening upon deployment.
Carotid Artery
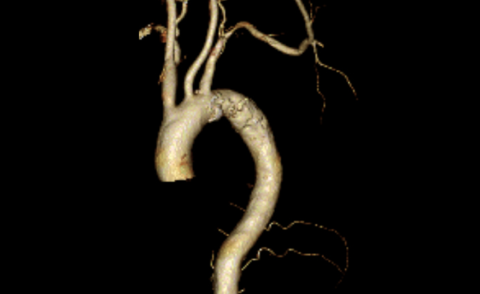
Subclavian Artery
We determined that as the stenosis location was distal to the origin of the vertebral artery, it would not pose a problem.
We began by inserting a 7Fr Glidesheath Slender, then advanced a RADIFOCUS Guide Wire M stiff type (J-tip) using a contrast catheter. At our facility, to minimize sheath movement during radial procedures, we use a combination of Glidesheath Slender and SlenGuide rather than Destination Slender for all cases. Upon encountering subclavian artery stenosis, angiography confirmed it was distal to the vertebral artery origin, so we proceeded with catheter advancement. We positioned the angiographic catheter (IMA shape) beyond the lesion, then advanced the SlenGuide to the lesion site while maintaining guidewire backup.
To determine the SlenGuide tip position, we employ a technique in which we retract the inner guide into the SlenGuide with the inner guide in place, inject contrast through the wire lumen of the inner guide to confirm position, and then remove it. This approach eliminates the need to reinsert the inner guide when adjusting the SlenGuide position.
We used a Misago stent for this procedure. After passing a floppy guidewire, we confirmed positioning with IVUS, performed pre-dilation, and then deployed the stent. The Misago stent's flexibility allows for good conformability in tortuous iliac arteries, facilitating easier positioning. Post-stenting, we confirmed results using IVUS and angiography before concluding the procedure (fig. 5).
Fig. 5: Procedure Details
a) Angiography of the subclavian artery
b) Catheter insertion (descending aorta)
c) Angiography of the lesion site
d) Stent deployment (Misago)
e) Angiography to confirm result
At our facility, we consistently use ultrasound guidance for all punctures to ensure accuracy, and we consciously opt for smaller diameter devices and sheaths whenever possible. We've incorporated DRA for vascular access, actively pursuing even less invasive treatment options.
While we implement R2P as one means of achieving less invasive EVT, ensuring safety is paramount when performing this procedure. To guarantee minimally invasive outcomes, we believe thorough preoperative evaluation, particularly of the access route, is critical.
*The author has received editorial fees from Terumo Corporation.